aka Hematology Hoodwinker 003
Emergency department management of the critically bleeding patient requiring massive transfusion is an area thats constantly changing and developing, making it difficult to keep up with what we should and what we shouldn’t be doing. The National Blood Authority has just released it’s first module Critical Bleeding/Massive Transfusion the first in a six module series based on patient blood management guidelines. These guidelines endorsed by the NHMRC, were created by a clinical reference group post extensive review of the recent literature surrounding the use of blood components in the management of patients with severe bleeding.
So enough of the boring stuff its time to put the guideline’s to the test with the ever popular LIFTL Q&A style post!!!
Case Study
It’s 3am Monday morning when a 23 male is brought in with multiple small calibre gun shot wounds to his back and chest.
His current vital signs are:
- Pulse: 127
- BP: 78/32
- Spo2 91 on 15 o2 via NRBM
- RR 11
- GCS 13/15 (E3, V4, M6)
You obtain a quick blood gas which shows the following:
- pH 7.14
- P02 74
- PC02 52
- HB 68
- Lactate 7
What are your initial priorities in managing this case? Is it time to start the massive transfusion protocol?
Questions
Q1. What are the definitions used to define “Critical Bleeding” and “Massive Transfusion”?
Critical Bleeding is defined as:
major haemorrhage that is life threatening and likely to result in the need for massive transfusion.
Broadly critical bleeding falls into 2 categories:
- Major haemorrhage that is life threatening and is likely to result in the need for massive transfusion
- Haemorrhage of a smaller volume in a critical area or organ (e.g. intracranial, intraspinal or intraoccular), resulting in patient morbidity or mortality
Massive Transfusion may be defined:
- In adults, as a transfusion of half of one blood volume in 4 hours, or more than one blood volume in 24 hours (adult blood volume is approximately 70mL/kg)
- In children, as a transfusion of more than 40mL blood/kg (blood volume of children older than neonates is approximately 80mL/kg).
Massive transfusion involves the administration of packed red blood cells, platelets and fresh frozen plasma on a 2.1.1 unit basis.
“Ultimately, the importance of defining critical bleeding or massive transfusion is to facilitate early recognition of this condition, or its potential, so that appropriate management can be instituted.”
Q2. What are the 5 common causes of critical bleeding?
- Trauma
- Gastrointestinal bleeding
- Ruptured aortic aneurysm
- Obstetric haemorrhage
- Surgical procedures
Q3. What should be evaluated for in the initial assessment of the critically bleeding patient?
Changes in physiological criteria can be important determinants in identifying critical bleeding, however avoid relying just on systolic blood pressure as a sole determinant of haemorraghic shock as this may result in a delayed recognition due to patients physiological compensating measures.
Initial assessment should include the evaluation of the following:
- History
- Systolic blood pressure
- Heart rate
- Pulse pressure
- Peripheral perfusion
- Mental status
- Respiratory rate
- Urine output
- Haemoglobin and haemocrit
- Coagulation status
- Acid-base status
- Temperature
Remember the patients physiological response will vary depending on the presence of the following:
- Age
- Cardiovascular disease (Hypertension, heart failure, pacemaker)
- Medications (Beta-blockers, Calcium channel blockers, Digoxin)
- Presence of hypothermia
Q4. What classification tool can assist you in classifying haemorrhagic shock in the critically bleeding adult patient?
The American College of Surgeons have created a tool to help you classify stages of haemorrhagic shock.
In clinical reality, the classification is not very useful — unless you’re trying to pass an exam or an ATLS course…
Learn more:
- Resus.ME — Evidence refutes ATLS shock classification
Q5. What is permissive hypotension and minimal volume resuscitation?
Past management practices for haemorrhagic shock involved aggressive fluid resuscitation with crystalloid solutions to achieve and maintain a near normal blood pressure. Unfortunately this lead to following complications occurring:
- Oedema, compartment syndrome and acute lung injury
- Exacerbation of anaemia, thrombocytopenia and coagulopathy due ti haemodilution
- Exacerbation of bleeding due to possible clot disruption
Following research showing these complications the concept of permissive hypotension and minimal volume resuscitation was developed and dates back to being used during World War II in the resuscitation of victims of combat.
“Permissive hypotension and minimal volume resuscitation are strategies in which systolic blood pressures of 80-100 mm Hg are tolerated while bleeding is being controlled.”
Permission hypotension is generally employed in the management of ruptured abdominal aneurysms, however is contraindicated in the management of traumatic brain injury as it will reduced cerebral perfusion pressure and oxygenation further leading to secondary brain injury.
Q6. What is the concept behind damage control surgery?
“Damage control surgery refers to the timely use if a staged approach in the treatment of the actively bleeding shocked patient.”
This approach emphasises control of bleeding and prevention of further contamination, to allow correction of hypothermia, coagulopathy and acidosis before definitive surgery is undertaken.
There are five critical decision-making stages in damage control surgery:
- Early patient selection
- Abbreviated life-saving surgery
- Secondary resuscitation
- Deferred resuscitation
- Reconstructive surgery, if required.
Damage control surgery works to help minimise/prevent the lethal triad:
Q7. Which biochemical values require monitoring in the critically bleeding patient?
In patients with critical bleeding requiring massive transfusion, the following parameters should be measured early and frequently:
- Temperature
- Acid-base status
- Ionised calcium
- Haemoglobin
- Platelet count
- PT/INR
- APTT
- Fibrinogen level
Values trending towards normal will indicate successful management of the critically bleeding patient.
Values indicating critical physiological derangement include:
- Temperature <35
- pH <7.2, base excess >-6, lactate >4mmol/L
- Ionised calcium <1.1mmol/L
- Platelet count <50 x 10/L
- PT > 1.5 X normal
- INR >.1.5 X normal
- Fibrinogen level <1.0g
- APTT <1.0g/L
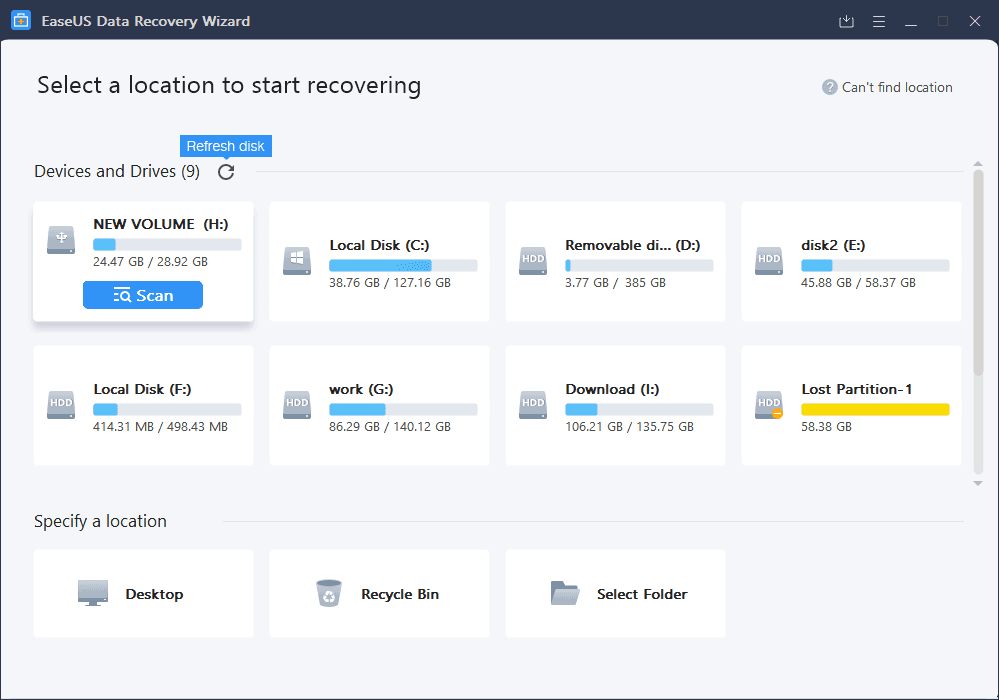
Q8. When should activation of the massive transfusion pack occur?
The following flow charts can be used as a guide to assist you:
When to organise the massive transfusion pack:
Suggested criteria for activating the massive transfusion pack:
Q9. What effect does dose, timing and ratio of component therapy have on patient outcomes?
Although the jury is still out on what is the optimum timing ratio for PRBC, FFP and Platelets, most studies have shown significant improved survival rates in patients receiving 2, 1,1, some studies and author’s recommend doing 1,1,1 in patients requiring massive transfusion. Further studies are needed before a recommended target ratio for PRBC, FFP, and platelets can be given.
Remember:
- Blood component replacement should be guided by clinical assessment and results of coagulation tests.
Optimum management requires prompt action, as wells good communication and coordination between treating clinicians, diagnostic laboratories and the transfusion service providers.
Q10. What are the recommendations for using Tranexamic Acid in the critically bleeding patient?
Although the guideline reviewers did not specifically address the effect of antifibrinolytic therapy in critically bleeding patients requiring massive transfusion. The reviewers felt it necessary to included the data from the recently published CRASH2 Trial , that showed improved survival in trauma patients that received tranexamic acid.
What is Tranexamic Acid?
- It is an antifibrinolytic that competitively inhibits the activation of plasminogen to plasmin, a molecule responsible for the degradation of fibrin.
When should I give Tranexamic Acid?
- Tranexamic acid should be considered in patients with,or at risk of, significant haemorrhage.
- The guideline reviewers make particular not to the fact that Tranexamic acid should be used as an adjunct in the critically bleeding patient, not as a ‘magic bullet”
What dose of Tranexamic Acid should i use?
- Loading Does 1g over 10mins
- Followed by infusion of 1g over 8 hours.
Learn more about tranexamic acid:
- EMCrit Podcast 67 – Tranexamic Acid (TXA), Crash 2, & Pragmatism with Tim Coats
- Emergency Medicine Literature of Note — Critique of Crash-2
- Emergency Medicine Ireland — Crash-2
- ICU Rounds Podcast — EARLY use of Tranexamic Acid may improve survival from bleeding in trauma
- Resus.ME — How about pre-hospital tranexamic acid?
- Resus.ME — Tranexamic acid saves lives in trauma
- The Lancet — Crash-2: Tranexamic Acid and Trauma Patients (includes link to fulltext pdf)
- The NNT — Tranexamic acid for Trauma
What more on managing the critical bleeder?
Listen to these podcast from EMCrit
The post Managing the Critical Bleeder!! appeared first on Life in the Fast Lane medical education blog.